TMJ Physiotherapy and Temporomandibular Disorders
Taking care of the temporomandibular joint is essential for relieving jaw pain, reducing muscle tension, and restoring function when speaking, chewing, or yawning.
I was very happy with the results
·
The best services I have ever experienced. Simply amazing!
·
Everything went very well. São super simpáticos e atenciosos.
·
When the jaw starts to rule
If your jaw hurts, clicks, locks, or if you feel constant tension in your face, it’s easy to ignore it for weeks. Until the day when chewing becomes uncomfortable, yawning seems like a challenge, and talking for long periods of time starts to tire you out. When this happens, your body is usually asking for one simple thing: less strain and more control on the temporomandibular joint.
What is really happening
Temporomandibular dysfunction does not appear by chance. It often stems from small habits that we repeat without realizing it: clenching our teeth, chewing on one side only, accumulated stress that ends up in the jaws, neck posture that is always tense, or a more difficult adjustment during orthodontic treatment. The result tends to be predictable: overworked muscles, less fluid movement, and pain that keeps coming back. At Clinicalvor, physical therapy for temporomandibular disorders looks at the problem holistically. We don’t just treat the spot where it hurts. We look for the pattern that is maintaining the tension and stiffness, so that the improvement is not just temporary relief, but a consistent change in how your jaw functions in your daily life.
What makes Physiotherapy different
The goal is clear and practical: to be able to chew, talk, and yawn again without thinking about it. To stop your jaw from being a constant issue. To achieve this, treatment focuses on three areas: relieving muscle tension, improving mobility, and training movement control to reduce relapses. Throughout the sessions, it is common to feel a progressive difference in the feeling of heaviness in the face, tiredness when chewing, and stiffness when opening the mouth. In many cases, there is also improvement in complaints associated with muscle tension, such as headaches and discomfort in the temple area. When orthodontic treatment is involved, physical therapy can help make the adjustment more comfortable, especially when phases of greater tension or sensitivity arise.
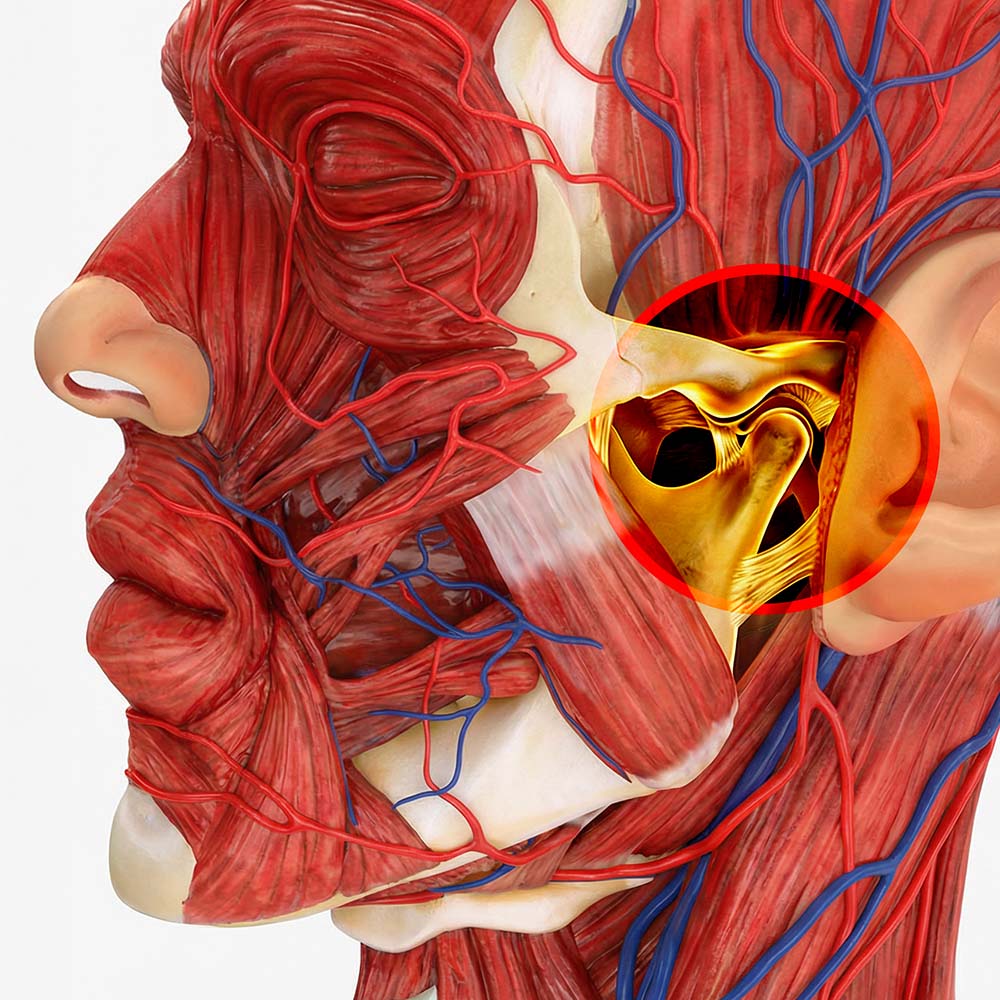
Temporomandibular Joint
The temporomandibular joint (TMJ) is the structure that connects the jaw to the temporal bone of the skull, located just in front of each ear. It is considered one of the most complex joints in the human body, as it allows hinge movements (opening and closing) and sliding movements (sideways and forward).
What you can expect to feel throughout the process
We begin by understanding your history: what you feel, when it started, what makes it worse, what relieves it, and what habits may be increasing the load on the joint. Then we assess the movement of the jaw, how it opens and closes, whether there is any deviation, limitation, muscle sensitivity, or signs of overload. Whenever it makes sense, we also assess your neck and functional posture, because the system works together and the jaw rarely works alone. If there are signs that indicate the need for evaluation by a dentist or other specialist, this is part of clinical rigor and your care, without beating around the bush.
Treatment
The treatment combines specific techniques to reduce tension and pain, exercises to improve coordination and stability, and simple everyday strategies that help reduce tightness and strain on the joint. No unnecessary force, no jaw manipulation. The focus is on function and comfort, with progression tailored to your individual case.
Quando este serviço faz sentido
This monitoring tends to help when there is pain when chewing or yawning, discomfort when clicking, a feeling of jaw fatigue, limited mouth opening, episodes of locking, frequent facial tension, or headaches that appear during periods of increased tightness. If you wake up with a heavy face, or if you notice that stress is affecting your jaws, it is worth evaluating.
Signs that warrant prompt evaluation
If there is sudden blockage with great difficulty in opening the mouth, recent trauma, marked swelling, fever, numbness, progressive severe pain, or neurological symptoms, the priority is clinical medical and/or dental evaluation before proceeding with functional intervention.
Action
If you want to understand what is causing the pain and what is keeping it there, book a physiotherapy assessment for temporomandibular disorders at Clinicalvor. We will provide a clear functional diagnosis and a plan with concrete steps to restore comfort, control, and peace of mind in your daily life.
TMDs are changes in the temporomandibular joint (TMJ) and/or chewing muscles that can cause jaw pain, facial tension, clicking, limited mouth opening, a feeling of jaw fatigue, and sometimes discomfort in the temples. There is not always a single cause. It is often a combination of muscle overload, clenching, repetitive habits, and less efficient movement patterns.
Not always. A popping sound can occur due to changes in joint and muscle coordination and may exist even without pain. The warning sign is not the sound itself, but rather the combination of pain, blockages, limited range of motion, feeling of instability, or progressive worsening. The goal of the evaluation is to determine whether the popping is just a “functional noise” or if there is a pattern that is increasing the load and warrants intervention.
In many cases, yes, especially when muscle components and movement control play a role in the problem. Physical therapy helps reduce tension and pain, improve controlled mobility, and re-educate opening and chewing patterns to reduce relapses. If there is a more specific joint component, the approach may include additional strategies and, when necessary, coordination with dental medicine.
It depends on your case and the type of TMD. A mouthguard can be useful in some situations, especially for dental protection and reducing nighttime overload, but it does not replace functional training, motor control, and daytime habit management. In many cases, the best strategy is a combination of physical therapy for function and musculature, and dental intervention when clinically indicated. At Clinicalvor, the assessment serves precisely to clarify what makes sense in your case.
It varies depending on the duration of symptoms, the intensity of pain, the presence of blockages, and everyday stress factors. Some people notice relief in the first few sessions, while others need more time to consolidate mobility and control. The most important thing is to have a plan with progression and strategies for home, because the best results appear when the work done in the consultation is continued in everyday life, with simple and consistent adjustments.

Joana Ulpiano
Physiotherapist
All dental services at your disposal
Clinicalvor has qualified technicians in various areas and state-of-the-art equipment that enables it to respond to any situation












